Cervical Spine: Structure, Disorders & Treatments Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief The cervical spine, commonly referred to as the neck, consists of 7 bones labeled C1 to C7 vertebrae. These bones are cushioned by intervertebral discs that not only enable the neck to move smoothly but also serve as shock absorbers during physical activities. As an upper cervical chiropractor, I work almost exclusively with the C1 and C2 vertebrae. However, I’ve studied the entire cervical spine extensively and worked with patients on issues with all of the vertebrae in that area. You might become aware of your cervical spine as you stretch before a workout. Or perhaps you notice if tension has collected in that area before a chiropractic adjustment . What is the cervical spine ? The cervical spine, or the C spine, is the neck part of your spine that protects your spinal cord and helps you move your head around. Taking care of it is crucial for your overall well-being. The cervical spine is composed of smaller articular bones. Articular means the bones are connected by joints, making it the most flexible region of the spine. Because of this mobility, the cervical spine can be more susceptible to injuries and disorders. We’re here to help you understand and care for your cervical spine, so you can keep moving and feeling great. If you have any questions, don’t hesitate to ask. Your spine is in good hands! If you’re in the Denver area, schedule an appointment with DUCC by calling us at 303-955-8270 or by visiting our Contact Us page. Cervical Spine Anatomy The spine can be divided into 5 regions : the cervical spine, thoracic spine, lumbar spine, sacrum, and coccyx. The cervical spine is comprised of 7 small bones labeled from C1 to C7, connected by discs to form the structural foundation of your neck. Housed within this neck structure is your spinal cord, shielded by bone and layers of protective meninges. Your cervical spine includes essential nerves that extend to your neck, shoulders, arms, and hands. Muscles and ligaments provide the necessary strength and stability to keep everything in place. That’s a general overview; now, let’s discuss each part for an in-depth understanding. The anatomical parts of the cervical spine include: 7 Cervical Vertebrae The cervical vertebrae C1-C7 connect the base of the skull to the top of the back. These vertebrae are the smallest vertebral bones in the spinal column. They form a lordotic curve (a curve towards the front of the body). C1 and C2 (the atlas and axis) are called atypical vertebrae because they function quite differently than C3-C6, which are called the typical vertebrae. Then there’s C7, known as the unique vertebra. It bridges the cervical and thoracic spine. Atlas and Axis The atlas (C1) and axis (C2) are the top 2 vertebrae that can be found just beneath the skull. They form the craniocervical junction and they allow all range of motion for the head and neck. The atlas (C1) is named for the mighty Titan, Atlas. In Greek mythology, he rebels against Zeus and is sentenced to bear the weight of the heavens. Similarly, the vertebral atlas sustains the weight of the cranium and brain. The atlas is referred to as a cradle because it cradles the skull. The axis (C2) has a vertical bony protrusion known as the dens or odontoid process. The ring-shaped atlas fits over the dens, creating the medial atlanto-axial joint, allowing the head’s rotational movement. Atlanto-Occipital Joint The atlas anchors the occipital bone (base of the skull) to the spinal column via the atlanto-occipital joint. This joint allows for much of the forward and backward motion of the head. Spinous Process Each vertebra has a bone extension called the spinous process (the ridge you feel through the skin extending the length of the back), where muscles and ligaments connect. Cervical Discs In between the cervical vertebrae are cervical discs. They cushion the vertebrae and function as shock absorbers between the bones during daily activities. These intervertebral discs consist of a tough outer layer called the annulus fibrosus and a soft interior called the nucleus pulposus. Vertebral Endplate Between each vertebra and disc, the vertebral endplate helps transfer nutrients from the bone to the disc. Spinal Canal Each vertebra consists of a vertebral body and vertebral arch. The anterior vertebral arch, made up of 2 laminae and pedicles, encloses each vertebra. Vertebrae are connected via the facet joints, enabling flexion (forward and backward motion). Together, the vertebral body and arch form an enclosed space called the vertebral foramen. The stacked vertebrae with their foramina (plural of foramen) create a tunnel called the vertebral column or spinal canal, which contains the spinal cord. Put in simpler terms, each bone in your spine has a curved bony part in the back. These curves join together to make a long hollow tunnel that goes through your whole spine. We call this tunnel the spinal canal. It’s like a pathway for your spinal cord and bundles of nerves. Spinal Cord The spinal cord is the central structure within the spine that runs from the base of the brain to the lower back, responsible for transmitting signals between the brain and the body. It plays a crucial role in transmitting signals for movement, sensation, and various bodily functions. Your spinal cord is cushioned by cerebrospinal fluid (CSF) and wrapped in 3 protective layers called the meninges. The meninges consist of the dura mater, arachnoid mater, and pia mater. Foramina At each level of your spine, a pair of tiny openings called foramina let nerves come out. There’s one opening on the left and one on the right. Cervical Nerves Cervical nerves are specific branches of spinal nerves that emerge from the foramina in the cervical or neck region of the spinal cord. Each cervical nerve has a particular role in controlling different areas of the upper body, such as the neck, shoulders, arms, and hands. Vertebral Arteries Laced throughout the cervical spine are vertebral
Cervical Instability: Causes, Symptoms, & Treatments
Cervical Instability: Causes, Symptoms, & Treatments Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief Cervical instability is a medical condition in which loose ligaments between the upper cervical spine and the base of the skull may lead to neuronal damage. Full disclosure from my years of experience treating patients with chiropractic care: This condition is massively over-diagnosed. However, I consider it with people suspicious of hyper mobility issues or with headaches and disequilibrium issues. When I suspect cervical instability in a patient, I take a lateral flexion anterior to posterior open mouth x-ray — that’s the best way to visualize it. If you have cervical instability, you may experience migraines, vertigo, or nausea, among other adverse symptoms. Fortunately, this condition is treatable. Let’s talk about the symptoms, causes, treatments, diagnosis, and prevention of cervical instability. What Is Cervical Instability? Cervical instability occurs when the ligaments in between your spinal cord and skull are loose. These “lax ligaments” allow for excessive movement of the top two cervical vertebrae, which may result in many symptoms, such as headaches, fainting, or even memory loss. Ligament laxity is a state in which ligaments that attach bone to bone are loose. Also called ligamentous laxity, this condition often causes chronic pain. It can affect the whole body, or only specific parts. You may have seen a friend hyperextend their finger, seemingly unnaturally. This is probably due to ligament laxity causing joint hypermobility syndrome. The ligaments connecting the bones in your friend’s finger are loose and allow for more range of motion. This abnormal range of motion in your neck area can trigger cervical instability. Ligament laxity may be caused by genetic connective tissue disorders, such as Ehlers-Danlos Syndrome or Marfan Syndrome. There are 2 joints at which the ligaments may be loose, leading to cervical instability: Atlanto-occipital joint Atlanto-axial joint Cervical instability is related to: Craniocervical instability Craniovertebral instability Clinical instability of the cervical spine Cervical neck instability Cervical spine instability Atlantoaxial instability What’s the difference between craniocervical instability and cervical instability? Craniocervical instability (CCI) and cervical instability are related concepts, but they refer to distinct conditions involving different parts of the spine and skull. Craniocervical instability involves the junction between the base of the skull (the occiput) and the top of the cervical spine (the first cervical vertebra, C1, also known as the atlas). Cervical instability involves the cervical spine, which is the neck region of the spine. It involves the vertebrae and ligaments and can affect the spinal cord and nerve roots in the neck area. Cervical Instability Symptoms Symptoms of cervical instability often include pain, weakness, numbness, and tingling. More severe neurological deficits may also present such as difficulty with coordination or loss of bladder or bowel control. Other cervical instability symptoms that may occur include: Feeling that your skull may “fall off” the spine Occipital headaches Migraines Muscle spasms Neck, shoulder , or jaw pain Difficulty swallowing Tenderness at the base of thee skull Light sensitivity Blurred vision Tinnitus (ringing in the ears) Orthostatic intolerance Tremors Vertigo Dizziness Clumsiness Fainting Limb weakness Shortness of breath Nausea Fatigue Lhermitte’s sign Cognitive decline Memory loss Loss of bladder or bowel control Trigeminal Neuralgia Cervical spine instability may lead to compression of the spinal cord or nerve roots in the cervical region. This compression can affect the function of the spinal cord, which is an extension of the brain stem. Abnormal pressure exerted on the nervous system may lead to a variety of neurological symptoms and impairments. Timely diagnosis and appropriate management are crucial to mitigate the impact on the nervous system and prevent further complications. Diagnosing Cervical Instability Diagnosing cervical spine instability can pose a challenge, often requiring the insights of a skilled orthopedic specialist to accurately detect. I can typically spot this problem in patients, but may refer them to an orthopedist to accurately diagnose if that can help open more treatment modality options. How do you test cervical instability ? The 4 methods for testing cervical instability include: Upright MRI: Magnetic resonance imaging Supine MRI: Laying on your back CT scan : Computerized tomography Digital motion x-ray As I stated earlier, I’ve found that a lateral flexion anterior to posterior open mouth x-ray is the most accurate diagnostic tool for proper visualization of this issue (if it exists). Abnormalities in the following measurements indicate cervical instability: Clivo-Axial Angle: Less than or equal to 135 degrees Grabb-Oakes measurement: Greater than or equal to 9 mm Harris measurement: Greater than 12mm Spinal subluxation : Any amount MRIs are the most common diagnostic testing method for cervical instability. A 2012 scientific investigation found that MRIs had limited diagnostic value in patients with whiplash-associated disorders such as cervical instability. Causes of Cervical Instability Cervical instability is caused by anterior and posterior ligament laxity between the skull and the top two vertebrae (the atlas and the axis ). This allows excessive movement and leads to a long list of physical and neurological symptoms. Causes of cervical instability may include: Whiplash or other injury causing rapid flexion/extension (such as from a car accident) Tethered cord syndrome Genetics Connective tissue disorders (such as Ehlers-Danlos Syndrome or rheumatoid arthritis) Chiari malformation Degeneration Treatments for Cervical Instability There are 5 standard treatments for fixing cervical instability: 1. Chiropractic Chiropractic care is a common and effective treatment for headaches , poor posture, and spinal misalignments — all of which are connected to cervical instability. Upper cervical chiropractic care may correct cervical instability. This 2020 study demonstrated how spinal chiropractic manipulative therapy can be used to correct cervical instability, joint disorders, dislocations of cervical vertebrae, and much more. Spinal manipulation is a safe and effective therapy when performed by a highly qualified chiropractor, even in special needs patients. Chiropractic treatment should always be considered before you move on to surgery. Note: Non-surgical spinal decompression therapy is not recommended for patients with cervical instability. Gentle adjustments of the upper spine are critical to recovering from cervical instability . Denver, CO residents can receive treatment with us at Denver Upper Cervical Chiropractic . Call us at 303-955-8270 to schedule an appointment. 2. Surgery Does cervical instability require surgery? You do not need surgery for cervical instability unless your instability has gotten
No, Chiropractic Adjustments Do Not Cause “Toxic Release”
No, Chiropractic Adjustments Do Not Cause “Toxic Release” Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief “Toxins” is a vague word that doesn’t really mean anything. Chiropractic adjustments greatly improve your body’s natural healing abilities, but there is not a specific toxin release that will make you feel sicker or healthier after an adjustment. Chiropractic care corrects spinal misalignment and subluxations, leading to a stronger nervous system and improved overall health. Chiropractic care does not correct body toxicity , which is a vague and dubious concept in the first place. However, chiropractic adjustment may strengthen the nervous system’s communication with the liver or kidneys, which both naturally detoxify the body. Strengthening these detoxing organs may help get rid of toxins, such as ammonia and uric acid. If your chiropractor employs a lot of massage techniques, that muscle fiber activation may lead to some temporary dehydration, which can lead to a slight feeling of illness if you don’t hydrate well afterwards. When I’m seeing patients, I’m honest with them. I’m a chiropractor, not a new age detox guru. Upper cervical chiropractic already heals people in surprising, evidence-based ways. Toxin release is unnecessary for the healing process, and I doubt it’s actually a thing. If you want a chiropractor who will be honest with you while using conservative, non-pharmaceutical treatments when possible, schedule your appointment with me at Denver Upper Cervical Chiropractic today. You can call us at 303-955-8270 . What Are “Toxins,” Anyway? Toxins are harmful substances that can make you sick in a variety of ways. However, the word “toxin” is so vague and all-encompassing that it loses all meaning when cited by many “health” influencers. In theory, releasing toxins through chiropractic adjustment or other means can make you feel groggy in the short-term then healthier in the long-term. I disagree with this theory — it’s not based on observable, definable, replicable research. Here’s a list of “toxins” that many chiropractors claim can released by chiropractic care: Polychlorinated biphenyls (PCBs) Chlorofluorocarbons (CFCs) Histamine Lactic acid Artificial preservatives Inorganic pesticides Industrial chemicals Heavy metals Air pollutants Do chiropractic adjustments really release toxins? No, chiropractic adjustments don’t really release toxins. Some claim the crack in your back is toxic release, which is untrue. I share the list above so you can do your own research — scientific study does not support the idea that any of those compounds are “released” by chiropractic adjustments or any form of spinal manipulation. In fact, if something leaks from your spinal cord, you probably need to visit an emergency room — because that something is spinal fluid, and you have an injury. Scientific Evidence for Body Toxicity The scientific evidence for “body toxicity” is next to none. In my educated opinion, the few instances of body toxins that could actually make you sick would benefit from using the specific toxin’s name, not the vague term “toxin.” It’s likely true that your body is exposed to various chemical compounds in your everyday life that make your body less healthy. However, every person is different, and every toxin is different. Calling them all “toxins” is unhelpful and medically meaningless. Chiropractic care improves your whole body health by correcting spinal misalignment , which strengthens your nervous system and even treats many kinds of headaches. But chiropractic adjustments don’t directly release toxins. Endotoxemia is a measurable variety of body toxicity which may warrant further research. Diet-induced systemic bacterial endotoxemia may result from consuming high amounts of sugar, flour, and oils. Healthy diet and healthy lifestyle can prevent endotoxemia. You May Feel “Sick” After an Adjustment Most people don’t feel “sick” after an adjustment, but some report fatigue and soreness. These symptoms are uncommon but natural and temporary, requiring a short adjustment period. Why does my body feel weird after a chiropractic adjustment? If your body feels lightheaded after a chiropractic adjustment, it’s probably due to a large change in the stimulus from proprioceptors and your body recalibrating to the new position of the corrected spine. In my experience, chiropractic patients don’t feel sick after an adjustment. If the rare occurrence they feel sore, lightheaded, or fatigued, it certainly has nothing to do with toxins. What are the symptoms of toxic release after chiropractic adjustment ? According to some, the side effects of toxic release after a chiropractic adjustment may include: Headache Fever Fatigue Nausea Dizziness Night sweats Sore or tight muscles Abdominal distress Flu-like symptoms What About Feeling Sick after Massage Therapy and Exercise? I’ve had patients ask about the ill feeling they sometimes have after massage or exercise, suggesting this is the same thing they feel after getting adjusted. Exercise can make you sweat, which is one of your body’s built-in detoxification processes. Massage, however, just dehydrates you (which can cause that ill feeling). During massage therapy, patients experience relaxation, but not release of toxins. You can actually get dehydrated due to your connective tissue and muscle fibers being activated and exercised, drawing moisture from your body and dehydrating you from the inside. This is why massage therapists give you water and tell you to drink more than normal after your appointment. During exercise, sweat naturally gets rid of some toxins and waste products. Physical exertion also pumps the blood circulation, accelerating detoxification in the lymph nodes and kidneys. A 2022 study found that more heavy metal toxins were released in sweat after exercising versus sweat from a heat sauna, implying that sweat alone is not the answer. Visit a Chiropractor Who Uses Only Evidence-Based Treatments I’m Dr. Ty Carzoli, an upper cervical chiropractor who has helped hundreds of patients overcome back pain , neck pain, migraines , headaches , vertigo, range of motion, and even mental health conditions. I don’t do these through the nebulous practice of so-called “toxic release,” but through evidence-based chiropractic treatment. Find a chiropractor who uses techniques that will actually help with the concerns you have. Any healthcare clinician you see should be able to defend or explain their rationale with evidence and sound reasoning, not appeals to emotion, metaphysical explanations, or ambiguous and vague jargon. Take control of your whole-body well-being , and work with us on a treatment plan that works for your unique situation. Schedule your appointment with Denver Upper Cervical Chiropractic right away. We are open on Friday but reserve that
What Is Orthospinology? Benefits, History, What to Expect & More
What Is Orthospinology? Benefits, History, What to Expect & More Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief Orthospinology is a subspecialty of chiropractic healthcare targeted to the top two vertebrae of the spine. Fixing misalignments in your upper cervical spine may address many underlying health problems , including seizures, chronic migraine, Parkinson’s disease, multiple sclerosis, high blood pressure, and more. At Denver Upper Cervical Chiropractic , we employ the evidence-based techniques of orthospinology to bring relief to patients who have found little success with man-made medications or want to avoid invasive surgeries. Listen to real customer testimonials about how upper cervical chiropractic care worked for them. Read below for more on orthospinology, including what it treats and what to expect from a visit to your qualified orthospinology chiropractor. What is orthospinology? Orthospinology is a gentle chiropractic technique that aligns the upper cervical spine (top two vertebrae) to reduce pain, promote overall wellness, and relieve chronic health conditions. Orthospinology is a conservative alternative to pharmaceuticals or surgery. This subspecialty of chiropractic care focuses on the upper cervical spine, which consists of the upper 2 vertebrae: The atlas , or C1 The axis , or C2 Upper cervical chiropractic care is gentle, not rough. We are not trying to ‘crack your back;’ we are fixing how your upper spinal cord communicates with your brain stem. This is what sets orthospinology apart from other chiropractic care. Orthospinology vs. NUCCA vs. Atlas Orthogonal National Upper Cervical Chiropractic Association (NUCCA) defines and regulates the practice of manually adjusting the upper cervical vertebrae based on x-ray analysis. This practice is slightly different from orthospinology. What is the difference between NUCCA and Orthospinology ? NUCCA adjustments are usually done by hand, but orthospinology procedures use instruments. A patient with good outcomes at a NUCCA office will typically have good outcomes at an orthospinology practice, and vice versa. Atlas Orthogonal is a little different from orthospinology though they are both upper cervical low-force procedures. The Atlas Orthogonal technique looks much like an orthospinology adjustment, but the instrument delivers the adjustment with a “percussive force” — essentially, a sound wave. Orthospinology techniques utilize a similar percussive instrument for some types of misalignments, but a larger table mounted instrument with a mechanical excursion for more. History of Orthospinology In the 1940s, Dr. John F. Grostic developed the Grostic technique — the beginnings of orthospinology. The Grostic technique focused on optimizing: Analysis specificity — making sure diagnostics accurately identify the underlying problem Adjustment precision — making sure chiropractic treatment precisely targets the underlying problem In the 1970s, Dr. John D. Grostic continued his father’s research. He expanded the list of upper spinal misalignment’s adverse effects on the central nervous system, based on overwhelming evidence. Orthospinology was born from the Grostic technique. Clinicians sought to improve the reproducibility of adjustments while minimizing human error with gentle, precise instruments. What causes neck misalignment? The following events may cause neck misalignment: Poor posture, including during sleep or work Traumatic spine or head injury (sports injuries, motor vehicle accidents, falls) Repeated “minor” injuries to the spine (chronically wrong lifting, staring down at phones) A long, stressful labor What causes atlas subluxation ? Traumatic injury is usually what leads to Atlas Subluxation Complex — a subluxation in your top vertebra. Poor posture and repeated injuries are common risk factors that worsen atlas subluxation. What happens when C2 is out of alignment? When the C2 (axis) is out of alignment, you can expect pain, numbness, weakness, or even loss of bladder/bowel control. You should seek upper cervical chiropractic care to correct C2 misalignment and avoid chronic health problems or long-term complications. What to Expect During Orthospinology Treatment During the orthospinology treatment process, expect an initial consultation. On your first visit , upper cervical chiropractors may not administer an adjustment. Precise analysis and diagnostics are crucial to orthospinology, so chiropractors often take a few days to process results. At your initial consultation, your upper cervical chiropractor may do a physical exam, digital x-ray analysis, maybe even a cognitive exam. On your second visit , chiropractors will typically perform the first adjustment. Upper cervical adjustments are gentle. Forget about those rough twists and cracks. Orthospinology is gentle enough for children and grandmas alike. These adjustments are often instrument-assisted. Sometimes, the instruments will be handheld. Other times, the instruments are mounted on advanced equipment.This video helps you know what to expect from an orthospinology adjustment. https://vimeo.com/299982455?fl=pl&fe=shhttps://youtu.be/MtWUoA5tt-8?si=GoG2atiI-DyQ0uga At Denver Upper Cervical Chiropractic, we also have a post-adjustment room for patients to relax and cool down after spinal realignment. Our calming post-adjustment room contains: Zero-gravity chairs Weighted blankets Noise-canceling headphones with binaural beats Essential oil diffuser Gentle lighting In our offices, we may also recommend upper and lower back stretches to help with certain conditions. How long does it take to realign your spine? It takes one adjustment to start realigning your spine. The total number of visits needed for total realignment varies by case and depends on the condition of the patient. However, a handful of visits to your chiropractor every year are likely needed to maintain spinal alignment. The Orthospinology Technique: Before and After Spinal decompression therapy is typically not recommended for the following people: Before After Before-After These before and after pictures from www.orthospinology.org show an average individual and how misaligned their spine may be before a spinal correction. Another method upper cervical chiropractors use is analyzing functional leg length by comparing the patient’s heels before and after adjustments. Before After Benefits of Orthospinology Orthospinology aims to improve nervous system function, immune system function, body imbalance, and overall wellness. But what specifically do upper cervical procedures treat? According to peer-reviewed research and case studies, the possible benefits of orthospinology /upper cervical care include improving medical conditions such as: Lower back pain Neck pain Knee pain Headaches and migraines Seizures Scoliosis Fibromyalgia Multiple sclerosis Parkinson’s symptoms Bowel dysfunction Asthma Low blood pressure High blood pressure Immune dysfunction (including when related to HIV ) Tourette’s syndrome Cerebral palsy Autism spectrum disorder Orthospinology as a Subspecialty of Chiropractic Orthospinology is a subspecialty of the chiropractic profession. It takes many credit hours of additional education and certification before
The Atlas Bone & When You Might Need an Adjustment
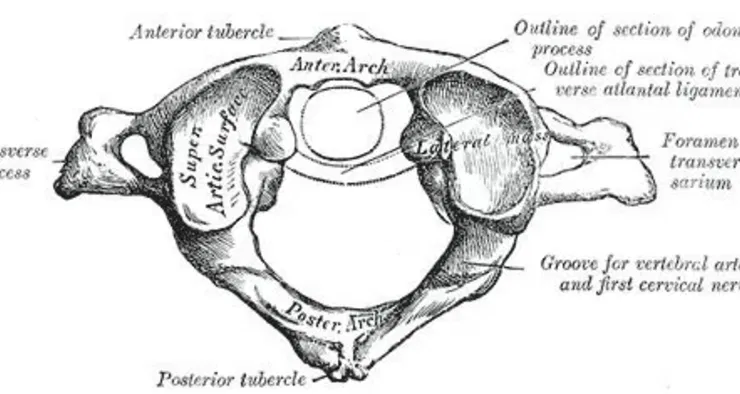
The Atlas Bone & When You Might Need an Adjustment Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief Much like the Atlas in Greek mythology who supported the entire world, the function of the atlas bone is critical: it supports your entire head. The atlas bone (C1) connects your skull to your spine, and — with the support of the axis vertebra (C2) just below — the atlas determines your head’s full range of motion. Misalignments in the atlas bone can cause chronic pain, stress, decreased range of motion, and tension in the head or neck. Keep reading to understand this critical vertebra and determine when a misaligned atlas may be causing you issues. From Anatomy, Head and Neck: Cervical Vertebrae (Public Domain) What Is the Atlas Bone? The atlas bone is the top bone or first cervical vertebra connecting your skull to your spine. It’s also known as the C1 vertebra in your cervical spine . Your whole spine has 7 cervical vertebrae that connect to the 12 thoracic vertebrae, which connect to your 5 lumbar vertebrae. Those lowest 5 vertebrae make up the lumbar spine and connect to the sacrum, then the coccyx at the base of your spine. Uniquely among vertebrae, the atlas vertebra at the very top of your spine lacks a vertebral body, spinous process, and the intervertebral discs found elsewhere in the spinal column. The atlas is a ring-like structure that joins the occipital bone above it with the axis, or C2 vertebra, below it — thanks to both the atlantooccipital joint and the atlantoaxial joint. These joints belong to a class of synovial joints that act as pivot points in the body. In this case, the pivot is your head movements. How does the atlas bone affect overall health? A misaligned atlas bone directly impacts headaches, migraines, neck pain, range of motion, and balance. A dysfunctional atlas may indirectly contribute to chronic pain, inflammation, brain fog, and mental health problems. Let’s dive into the atlas bone’s support structure and general anatomy to get a deeper understanding of how it works. Here are the major parts of your atlas bone: Lateral masses Transverse process Anterior arch Posterior arch Vertebral foramen Lateral Masses The lateral masses (Massa lateralis atlantis) of the atlas bone are its thickest and sturdiest parts, which is by design. The pair of masses support the weight of your skull. Superior and inferior facets, or small joints, are found on each side of the lateral masses. The superior articular facets on the superior surface connect to the occipital condyles on your occipital bone. These structures allow for neck flexion and nodding movements of the head. This part of your atlas allows you to nod your head “yes” — why the atlas is also called the “yes bone.” The inferior articular facets on the inferior articular surface allow articulation with the axis, or second cervical vertebra, and head rotations. Essentially, these facets are where the two joints meet. Transverse Processes The transverse processes are large projections from the lateral masses that attach to the muscles here and help you rotate your head and neck. These muscles include the rectus capitis lateralis, a small muscle important to lateral bending of the occiput, or the back of your head. The transverse foramen in the transverse processes is a hole for your vertebral artery. From Anatomy, Head and Neck: Atlantoaxial Joint (© 2024, StatPearls Publishing LLC) Anterior Arch The anterior arch is concave on one side and convex on the other. That shape allows it to work as a connecting segment for the odontoid process (dens) of the axis below and the transverse ligament. From above, it attaches the long muscle of the neck (longus colli muscles) with the anterior tubercle. The upper border of the anterior arch attaches to the anterior atlantooccipital membrane. The lower border attaches to the anterior atlantoaxial ligament and the anterior longitudinal ligament. Most importantly, these connections are a pivot point with the axis. Posterior Arch The thin posterior arch that ends behind the posterior tubercle makes up about two-fifths of the circumference of the atlas ring. The posterior tubercle sits at the apex of the posterior arch and serves as an attachment site for the nuchal ligament (ligamentum nuchae), which spans the 7 vertebrae of the cervical spine. A groove in the posterior arch allows the vertebral artery to pass through here and the foramen magnum and continue along the spinal column. Defects in this area that lead to interference between the atlas and your skull can cause neurological problems down the line if left untreated. Vertebral Foramen The vertebral foramen is a large opening in the bone for both the spinal cord and the odontoid process of the axis. On the axis side, it serves as the start of a pivot point for your C2 vertebra. Read Next: Trigeminal Neuralgia vs TMJ, What Are They? Atlas Misalignment Atlas misalignment may cause various health problems and impact the structural integrity of your spine over time. How does your atlas get misaligned? Your atlas can get misaligned due to injury, abnormalities in your bone structure , or a variety of conditions affecting the spine and musculoskeletal system. Poor posture can also cause atlas misalignment over time. One rare injury that directly affects the atlas is a Jefferson fracture, most often seen alongside spine or head injuries. Generally, atlas fractures are more common in the elderly. It can be difficult to know how many people have an atlas misalignment, as many patients don’t seek care immediately. Atlas misalignment is among the most common conditions addressed by chiropractic care. What are the symptoms of a misaligned atlas? The symptoms of a misaligned atlas include: Headaches Migraines Pain in the jaw, neck, and back, and muscle stiffness Hearing problems, e.g. tinnitus, hearing loss, inner ear conditions Shoulder pain or misalignment of the scapulae, or shoulder blade Restricted movement of the head up and down or side to side Dizziness, including vertigo Balance problems Difficulties with coordination and concentration Muscle spasms Pelvic and hip misalignment Trigeminal neuralgia
Spinal Decompression Therapy: Heal the Spine Naturally
Spinal Decompression Therapy: Heal the Spine Naturally Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief If you have persistent chronic pain in your back , neck , or hips, spinal decompression therapy may offer relief. This non-invasive therapy treats the root cause of your pain. This form of therapeutic traction is most helpful for people with disc degeneration, bulging or herniated discs, and radiculopathy (pain radiating into the arms or legs). Spinal decompression can help a significant percentage of patients without requiring surgery. This is especially helpful for patients with disc issues like loss of disc height that are traditionally treated with surgery alone. In our office, we’ve seen a significant improvement in pain for patients with disc problems, especially those whose spines don’t respond as quickly to chiropractic adjustments. It’s best when used over multiple sessions, and all of the feedback I’ve gotten is that it’s incredibly gentle and a great help. In fact, we invested in our own spinal decompression table just recently! Learn more about the benefits of spinal decompression below. What Is Spinal Decompression? Spinal decompression is a non-surgical therapy that may relieve back pain and promote the natural healing of the spine. Decompression therapy gently stretches the spine, creating a vacuum effect that helps retract herniated or bulging discs. It’s one of the only effective non-surgical treatment options for disc pain. A decompression table allows chiropractors greater precision in the target area, especially compared to an inversion table or other forms of traction that don’t let you dial in the tension applied or the region you’re applying tension to. This safe, painless process also enhances the flow of nutrients, oxygen, and fluids into the spinal discs, further facilitating disc healing and reducing pinched nerves. I find that patients whose spines are most stubborn to respond well to adjustments benefit most from spinal decompression. Spinal decompression should be performed by a qualified chiropractor. Do not attempt decompression at home. Your chiropractor may recommend targeted at-home stretches that are safe and helpful. “Spinal decompression” sometimes refers to surgical treatment , but non-surgical decompression therapy is not the same as surgical spinal decompression. Types of Spinal Decompression Therapy Below are the most common types of spinal decompression therapy: Motorized Traction — This method involves a traction table or similar device intermittently stretching and relaxing the spinal column. Chiropractors and physical therapists often use spinal decompression tables for the most precise results. Manual Spinal Decompression — This type is also performed by a chiropractor using instrument-free, hands-on techniques to stretch the spine. Surgery — Spinal decompression surgery may include removing vertebra bone (laminectomy) or spinal disc (discectomy). A surgeon may also fuse two vertebrae together with a bone graft. Back surgery is invasive and more dangerous than the other types but may be needed in severe circumstances. Our office at Denver Upper Cervical Chiropractic just invested in a new spinal decompression table for our patients. We are seeing incredible results in their quality of life! To schedule an appointment, call 303-955-8270. Benefits of Spinal Decompression Therapy According to recent research , the health benefits of non-surgical spinal decompression therapy include the following: Pain relief Increased range of motion More back muscle endurance Higher quality of life Fewer side effects compared to pharmaceuticals or surgery Conditions That Spinal Compression May Treat Non-surgical spinal decompression therapy may benefit these conditions: Chronic back pain Sciatica Spinal stenosis Herniated discs Degenerative disc disease Facet syndrome Symptoms of a Compressed Spine It’s vital to recognize the signs of compressed nerves and a compressed spine. If you’re experiencing any of the following symptoms, spinal decompression therapy may be beneficial for you: Chronic pain in the lower back , neck, or buttocks — Leg pain, neck pain, or back pain that doesn’t improve with conventional treatments Numbness or tingling — Sensations in the arms, hands, legs, or feet Weakness — Difficulty moving the affected parts of the body Reduced range of motion — Difficulty bending or twisting Read more: Can Chiropractors Relieve Occipital Neuralgia Pain? Common Causes of a Compressed Spine Below are the most common causes of compressed spine symptoms: Herniated or bulging discs — Discs protrude and press on spinal nerve roots when herniated or bulging Degenerative disc disease — The discs between the vertebrae lose their cushioning in this disease, leading to pain Poor posture — Posture misalignments put extra pressure on the spinal cord Back injury — Accidents, falls, and other injuries increase the risk of nerve compression and lumbar spine pain When to Discuss Surgery In certain cases, conservative treatments may fail to provide relief, and you and your doctor might consider different types of surgery. Here are the signs that orthopedic surgery should be discussed: Persistent pain — When non-invasive treatments have failed to improve your symptoms and quality of life Severe nerve damage — Evidenced by loss of sensation or weakness Loss of bowel or bladder control — Indicating cauda equina syndrome, a surgical emergency Surgery is rough on the human body and comes with side effects. Risks of surgery include: Infection Blood clots Bleeding Nerve damage Scarring Long recovery period Risks associated with anesthesia How to Prevent Spinal Compression If you prevent spine compression pain, you may not need expensive treatments. Preventing spinal compression includes adopting a holistic and proactive approach to spinal health. Below are ways to prevent spinal compression in the first place: Practice proper posture — Especially when sitting or lifting objects Regularly exercise — Strengthening the core muscles supports the spine Maintain a healthy weight — Reducing strain on the spine and back Invest in ergonomic workstations — Ensuring your work setup supports spinal health Seek professional guidance — Such as from a chiropractor or physical therapist When Spinal Decompression Is NOT Recommended Spinal decompression therapy is typically not recommended for the following people: Pregnant women Those with spine fractures or tumors Those with broken vertebrae Those who have undergone spinal fusion Those who have metal implants in their spine Those who have advanced osteoporosis Other treatments for negative pressure on spinal nerves include general chiropractic , acupuncture, and physical therapy. FAQs Is it good to decompress your spine? It is good to safely decompress your
Living in Limbo: Navigating Life with Undiagnosed Neurological Symptoms
Living in Limbo: Navigating Life with Undiagnosed Neurological Symptoms Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief The Frustration of Not Having a Diagnosis Living with undiagnosed neurological symptoms is a constant struggle, marked by a never-ending cycle of doctor visits, tests, and uncertainty. Individuals often experience symptoms that severely impact their daily lives, yet remain undiagnosed despite thorough medical evaluations. This can lead to feelings of frustration, helplessness, and even skepticism from healthcare providers. Common Unexplained Neurological Symptoms People suffering from unexplained neurological symptoms often report persistent headaches or migraines, muscle weakness or paralysis, numbness or tingling sensations, balance and coordination issues, cognitive difficulties such as memory loss or confusion, visual disturbances, and speech difficulties. Types of Unexplained Neurological Symptoms Chronic Headaches & Migraines : These can be debilitating, often occurring without an identifiable cause, leading to significant discomfort, nausea, and sensitivity to light and sound. Chronic migraines can disrupt daily life, making it difficult for individuals to maintain their regular routines. Peripheral Neuropathy: Involves damage to the peripheral nerves, causing pain, numbness, and weakness, particularly in the hands and feet. This condition can arise without a clear cause, leading to significant distress and functional impairment. Patients often describe the sensation as burning, tingling, or electric shocks. Unexplained Seizures: These can occur sporadically and are difficult to manage without a definitive diagnosis. Seizures without a known cause can be particularly challenging to treat, as they may not respond well to standard epilepsy medications. The unpredictability of these seizures adds to the patient’s anxiety and stress. Movement Disorders: Tremors, dystonia, or tics can occur without an identifiable cause, making them challenging to treat. These disorders can manifest as involuntary movements, muscle contractions, or repetitive motions, severely impacting a person’s ability to perform daily tasks. The lack of a clear diagnosis often complicates the management and treatment of these symptoms. Functional Neurological Disorder (FND): Patients experience neurological symptoms like limb weakness, seizures, or sensory disturbances without any structural or biochemical abnormalities. These symptoms can mimic serious neurological conditions but are not explained by traditional medical tests. FND can significantly impact a person’s quality of life and requires a comprehensive approach to diagnosis and treatment. Chronic Fatigue Syndrome (CFS): Characterized by extreme fatigue that does not improve with rest and cannot be explained by any underlying medical condition. Patients with CFS often experience additional symptoms such as sleep disturbances, memory issues, and muscle pain, which further complicate their condition. Autonomic Dysfunction: Involves the autonomic nervous system, leading to symptoms such as abnormal heart rate, blood pressure issues, and digestive problems. These symptoms can be severe and disruptive, occurring without a clear underlying cause. Cognitive Impairments: Includes issues with memory, attention, and executive function that are not linked to any identifiable brain injury or disease. These impairments can severely affect daily functioning and quality of life, adding to the frustration of living with undiagnosed symptoms. Sensory Disturbances: Patients may experience unexplained changes in sensation, such as numbness, tingling, or heightened sensitivity. These disturbances can affect various parts of the body and can be persistent or intermittent, complicating diagnosis and treatment. Diagnostic Challenges Exhaustive Medical History and Physical Examination: Despite thorough evaluations, a definitive diagnosis often remains elusive. Comprehensive Testing: Imaging studies (MRI and CT scans), EEGs, blood tests, and lumbar punctures frequently yield inconclusive results, adding to the frustration. The Emotional Toll The absence of a diagnosis can lead to significant emotional and psychological distress, including anxiety, depression, and a sense of isolation, as patients may feel dismissed or not taken seriously by healthcare providers. Managing Unexplained Neurological Symptoms Symptom Management Psychological Support Lifestyle Adjustments Medications such as pain relievers, antidepressants, and anticonvulsants can help manage symptoms. Pain relievers reduce discomfort, antidepressants address mood disorders and chronic pain, and anticonvulsants manage nerve pain and seizures. Physical therapy improves strength, coordination, and balance through tailored exercise programs and manual therapy techniques like massage. Cognitive Behavioral Therapy (CBT) helps patients manage symptoms by changing their thoughts and behaviors, addressing the psychological aspects of chronic pain. Support groups provide emotional support and practical advice, offering a sense of community and shared experience. Stress management techniques like mindfulness, meditation, and relaxation exercises can reduce symptom severity. Maintaining a healthy lifestyle through diet and exercise improves overall well-being, while avoiding triggers such as caffeine or alcohol and ensuring adequate sleep can significantly impact symptom management. Integrating these lifestyle changes leads to a holistic improvement in health and a reduction in the severity and frequency of neurological symptoms. Medications such as pain relievers, antidepressants, and anticonvulsants can help manage symptoms. Pain relievers reduce discomfort, antidepressants address mood disorders and chronic pain, and anticonvulsants manage nerve pain and seizures. Physical therapy improves strength, coordination, and balance through tailored exercise programs and manual therapy techniques like massage. Cognitive Behavioral Therapy (CBT) helps patients manage symptoms by changing their thoughts and behaviors, addressing the psychological aspects of chronic pain. Support groups provide emotional support and practical advice, offering a sense of community and shared experience. Stress management techniques like mindfulness, meditation, and relaxation exercises can reduce symptom severity. Maintaining a healthy lifestyle through diet and exercise improves overall well-being, while avoiding triggers such as caffeine or alcohol and ensuring adequate sleep can significantly impact symptom management. Integrating these lifestyle changes leads to a holistic improvement in health and a reduction in the severity and frequency of neurological symptoms. Neurological Factors Neurological dysfunctions play a significant role in unexplained chronic pain. Nerve dysfunction, where the nervous system abnormally processes pain, and central sensitization, where the central nervous system becomes highly sensitive, are key factors. These conditions amplify pain responses even in the absence of an ongoing injury or disease. Psychological Factors Stress and anxiety can exacerbate pain perception. Chronic stress can lead to muscle tension and pain, while anxiety can heighten the body’s pain response. Depression is another critical factor, as it can both result from and contribute to chronic pain. The interplay between chronic pain and depression often creates a vicious cycle that is
Staying Fit for Family Fun in Nature: How Chiropractic Littleton CO can Help Parents
Staying Fit for Family Fun in Nature: How Chiropractic Littleton CO can Help Parents Exploring the Unique Causes of Headaches in Denver and How Chiropractic Care Provides Relief Chiropractic Care in Littleton CO: Helping Parents Stay Active Living in Littleton, Colorado, offers families the best of both worlds—a family-friendly suburb with proximity to outdoor adventures. Whether you’re enjoying a day in South Platte Park or exploring the trails at Carson Nature Center, outdoor activities are a huge part of life here. For parents who want to keep up with their kids and explore Colorado’s great outdoors, staying physically fit is essential. Chiropractic care plays a significant role in helping parents maintain the strength and flexibility needed to keep up with Littleton’s active lifestyle. In this blog, we’ll explore how chiropractic care can help parents stay in peak shape, prevent injuries, and keep the whole family active and enjoying the beauty of nature. Keeping Up with Your Kids: The Challenge of Family Adventures Parenting is a full-body workout. Whether you’re pushing strollers, chasing after toddlers, or carrying gear for a family picnic, it’s no wonder many parents experience strain on their backs, necks, and joints. These physical demands can intensify when you’re navigating uneven terrain on hiking trails or spending long hours outdoors. The strain on your muscles and joints often leads to soreness or even injuries, making it harder to enjoy family activities. Chiropractic care can be a game-changer for parents, helping you stay fit, mobile, and injury-free. Regular adjustments realign the spine and reduce stress on muscles and joints, allowing your body to move more fluidly and handle the physical demands of parenting. Chiropractic care also helps to release tension built up from constant lifting, carrying, and bending over, keeping your body balanced. Keeping your body in optimal condition means more time exploring the outdoors with your family and less time dealing with aches and pains. At Denver Upper Cervical, we have all of the chiropractic specialties including rehabilitation, treatment for headaches, TMJ, post concussion syndrome and even vertigo! The Strain of Outdoor Adventures: How Chiropractic Can Help Littleton’s proximity to nature provides endless opportunities for hiking, biking, and camping. But the physical strain from these activities can take a toll on your body, especially if you’re not used to the challenges of rugged terrain. Hiking, in particular, puts strain on the knees, ankles, and lower back. Walking uphill can cause stress on the muscles and joints, and downhill hikes can increase pressure on your knees. Activities like hiking can exacerbate knee pain caused by overuse, improper footwear, or carrying heavy loads. Mountain biking, a popular outdoor activity in Colorado, is also associated with wrist fractures and shoulder dislocations from falls and impacts. Symptoms of wrist fractures include pain, swelling, and difficulty moving the wrist. When it comes to biking, poor posture and improper gear can also contribute to joint pain. Chiropractic care can help manage these injuries by promoting proper alignment, reducing pain, and speeding up recovery. Through regular chiropractic adjustments at Denver Upper Cervical, you can minimize the risk of repetitive strain injuries and keep your body in top condition. Shoulder dislocations, which often occur from falls while biking, require immediate care and rehabilitation. Chiropractic adjustments, combined with physical therapy, can help strengthen the shoulder and prevent future dislocations. Regular chiropractic care will help parents enjoy biking and other outdoor activities without the fear of recurring injuries. Preventing Common Injuries: Stay Active with Your Kids Outdoor adventures in Littleton are exciting, but they also come with risks of injury. Whether you’re hiking, playing sports with your kids, or biking on rugged trails, you’re bound to face physical challenges. Other common injuries, such as ankle sprains and knee pain, can easily occur when navigating uneven terrain during hikes or other outdoor activities with your kids. Ankle sprains are a common injury caused by overstretching or tearing the ligaments, often from stepping on uneven surfaces or sudden twisting motions. In active families, falls from mountain bikes or while hiking can also lead to wrist fractures and shoulder dislocations, especially if proper care is not taken. Chiropractic care is key to not only treating these injuries but also preventing them through improved joint stability and flexibility. By addressing the root causes of musculoskeletal problems, chiropractic care ensures that your body can recover quickly from minor injuries and remain resilient during physical activities. Regular chiropractic care can also promote better posture and alignment, which can reduce the risk of overuse injuries. Strengthening exercises recommended by our chiropractor at Denver Upper Cervical will also help reinforce weak joints and support long-term health. For parents who want to enjoy activities like mountain biking without injury, regular chiropractic care is essential for keeping joints and muscles in optimal condition. Family Wellness: A Holistic Approach to Outdoor Adventures At Denver Upper Cervical, we believe in a holistic approach to family wellness. This means focusing on your entire body’s health, from improving mobility to reducing stress and tension. Chiropractic care is more than just adjustments; it’s about supporting your overall health and well-being so that you can enjoy a full and active life with your family. By addressing misalignments in the spine and nervous system, chiropractic care enhances your body’s natural ability to heal, helping you remain active and energetic. Research shows that chiropractic care can support overall health by improving the nervous system’s function, enhancing your body’s ability to adapt to the physical demands of outdoor adventures. Our gentle, NUCCA-based chiropractic adjustments are designed to align the upper cervical spine, ensuring that your body can function at its best. We take a personalized approach, making sure that our care is tailored to the specific needs of each patient, helping you maintain long-term health and performance. With our focus on precise, gentle care, we help you maintain flexibility and strength while reducing pain and discomfort, allowing you to keep up with your kids in nature. What to Expect at Denver Upper Cervical When you visit Denver Upper Cervical, you can expect a personalized approach to your care. Your first appointment