Basilar Migraine: Triggers, Symptoms, Treatment & Prevention
Millions of Americans suffer from migraines every year, but one specific type of migraine comes with some trippy visual symptoms.
Basilar migraines are a strange phenomenon, not well understood in the conventional medical community. These migraines start in the brain stem and are preceded by an “aura,” which is a set of visual symptoms, like seeing flashing lights that are not actually there.
It can be important to recognize the symptoms of a basilar migraine as well as discuss the potential causes of this medical condition.
The pharmaceutical industry thrives on masking symptoms but leaving root causes untouched. That way, the underlying cause keeps causing problems, and you have to continue buying medication.
At Denver Upper Cervical Care,
our patients
actually get better. Each person’s body has the ability to heal — if we simply address the root cause.
Basilar migraines are a bit mysterious, but there are several known risk factors that you can reduce. You can also learn about the 16 best treatment options if you read below.
What are basilar migraines? Are they dangerous?
Basilar migraines are a migraine type that lasts about an hour and begins in your brain stem.
Scientists are not 100% sure what exactly the cause is. Many believe basilar migraines occur due to vasoconstriction, or the narrowing of blood vessels. The muscular wall of the vessel tightens and constricts blood flow.
These types of migraines are sometimes called basilar artery migraines because some believe that a spasm of the basilar artery
might be the main culprit behind these migraine attacks. Actually, this is a less and less common theory, and “basilar migraine” is no longer the recommended term.
What is a migraine with brainstem aura?
Migraine with brainstem aura is the most recent term recommended for use by the International Headache Society (IHS). However, both “basilar migraine” and “migraine with brainstem aura” can still be used interchangeably at this point.
An aura can be scary the first time you experience it. A typical aura occurs less than an hour before the head pain starts.
A migraine aura is a set of visual symptoms
that can accompany a migraine. All basilar migraines come with aura symptoms.
Basilar migraines are sometimes called Bickerstaff migraines, named after Edwin R. Bickerstaff who first identified
the condition in 1961.
Are basilar migraines dangerous?
This relatively rare type of migraine headache can
be dangerous. Basilar migraines seem to increase your risk of ischemic stroke, especially in women who take contraceptives.
Also, basilar migraines can decrease your level of consciousness or awareness. This means you don’t want to get a basilar migraine while you’re driving.
Symptoms of a Basilar Migraine
Although basilar migraines feature aura symptoms, which can be a little frightening, these symptoms of migraines with brainstem aura include more than just visual symptoms.
- Headache pain on one or both sides of your head
- Vertigo
- Lack of coordination
- Confusion
- Slurred speech
- Nausea
- Double vision
- Temporary loss of hearing, ringing in your ears
- Loss of muscle control
- Loss of consciousness
- Aura symptoms (last for about 20 minutes, occur
before
migraine):
- Seeing flashing lights
- Seeing spots, lines
- Seeing static
- Weakness, exhaustion
- Numbness in head, hands, or face
- Temporary vision loss
Diagnosis
There are several medical conditions easily confused with basilar migraines. A clinical diagnosis is very important to distinguish between a basilar-type migraine and a brain disorder.
The International Classification of Headache Disorders (ICHD) 3rd edition provides us with detailed diagnostic criteria :
- At least two migraine attacks (which fulfill 2 and 3 below)
- Aura, consisting of temporary visual/sensory/speech symptoms, but no motor or retinal symptoms
- At least two
of the following symptoms:
- Slurred speech (dysarthria)
- Double vision (diplopia)
- Temporary loss of hearing (hypacusis)
- Ringing in your ears (tinnitus)
- Loss of muscle control (ataxia)
- Numbness on both sides of your body (bilateral paresthesia)
- Vertigo
- Decreased level of consciousness
- At least two
of the following characteristics:
- At least one aura symptom over the course of five minutes
- Two or more aura symptoms occur in succession
- Aura symptoms last 5-60 minutes
- At least one aura symptom is unilateral
- The aura is followed by headache pain
- Transient ischemic stroke and other similar diagnoses have been ruled out
To rule out neurological diseases, you may need to see a neurologist. The neurologist may administer a magnetic resonance imaging (MRI) scan or computer tomography (CT) scan to rule out a number of brain disorders, or an electroencephalogram (EEG) to rule out seizures.
What conditions might your doctor want to rule out before treating you for migraines with brainstem aura?
- Stroke
- Epilepsy
- Meningitis
- Vestibular disorder
Basilar migraines are similar in nature to familial hemiplegic migraines. Hemiplegic migraines uniquely include weakness on one side of your body, as well as trouble speaking. A clear diagnosis will distinguish between the two.
Causes & Risk Factors
Scientists do not know exactly why basilar migraines occur. But there are certain risk factors that have been attributed to basilar migraine attacks:
- Stress (physical or emotional)
- Lack of sleep (or, in rarer cases, excessive sleep)
- Poor posture
- Motion sickness
- Alcohol
- Caffeine
- Dietary nitrites (like in hot dogs)
- Being overweight, obese
- Bright lights, flashing lights
- Seizures, epilepsy
- Blood pressure medications
- Medication overuse
- Hormonal contraceptives
- Hormone fluctuations (such as during menstruation, pregnancy, or menopause)
- Strong smells (such as cologne, perfume)
- Changes in the weather
Also, it is worth noting that basilar headaches are more prevalent in females than males. Though basilar migraines have been observed appearing for the first time in patients as old as 62, these migraines typically affect adolescents and young adults.
Are basilar migraines hereditary?
Typically, NO, basilar migraines are not inherited via genetic features.
However, in very rare cases, propensity towards basilar migraines can be due to a genetic mutation (in the ATP1A2
or CACNA1A
genes). In these rare situations, a parent has a 50% chance of passing that susceptibility of basilar migraines on to a child.
16 Treatment & Prevention Strategies
How do you stop basilar migraines? Your body is a robust system, more than capable of healing itself if you are able to identify and address the underlying issue.
While we figure out how to resolve the root cause of your basilar migraine, there are also some easy methods to find pain relief.
Always talk to your doctor before starting any new medication or major lifestyle changes.
Treating the Root Cause
- Stress relief may be critical to stopping your basilar migraines. If chronic stress is the root cause, then meditation , taking up a hobby, or spending time outdoors might help reduce your headache frequency.
- A full night’s rest might be what you’re missing. Since not enough sleep is a potential root cause, make sure to get seven to eight hours of quality sleep every night.
- A healthy diet can reduce migraine frequency. Avoiding nitrites, caffeine, and alcohol, as well as eating consistent meals can improve your overall health and avoid potential triggers for migraines. Also, overweight people are at higher risk of basilar migraines. Shedding those extra pounds may reduce the frequency and severity of your migraines.
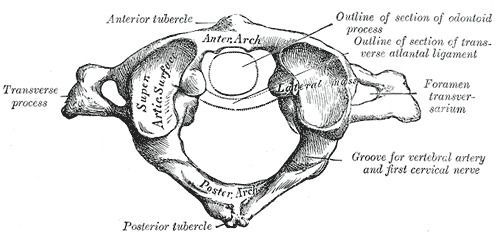
- Upper cervical chiropractic care is essential for your spine and neck alignment. Research supports chiropractic care’s ability to treat migraines. That alignment reduces the physical stress that can lead to migraines. We have helped so many people recover completely.
If you live in the greater Denver area, click here to request an appointment at Denver Upper Cervical Chiropractic. For your convenience, we reserve Fridays for out-of-town patients.
Symptom Prevention Strategies
- Botox injections (as often as every three months)
- Anti-seizure medication
- Antidepressants
- Blood pressure medication , such as beta blockers or calcium channel blockers, including topiramate or verapamil
Note: Blood pressure medications are also a potential cause of basilar headaches, so you should not rely too heavily on them.
Pain Relief Medication
- Triptans , a family of drugs developed for the acute treatment of migraine headaches
- Non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen
- Peripheral nerve blocks
- Anti-nausea meds , such as dramamine (because nausea is a common symptom)
Even though these will not prevent migraine attacks, you can take these symptom relievers as soon as you feel aura or migraine symptoms to prevent symptoms from spiraling out of control.
All-Natural Pain Relief
These all-natural headache pain relievers just scratch the surface. There are dozens of supplements and essential oils that may improve your symptoms while you treat the source.
Long-Term Prognosis
If you have basilar migraines, over-the-counter medication, rest, chiropractic care, and some simple lifestyle changes should relieve the headache pain.
However, if your migraine symptoms or aura symptoms make daily tasks difficult, see your doctor right away. If a migraine makes you lose consciousness, it is time to visit the ER.
- Charles, A. (2018). The migraine aura. Continuum 24 , 1009-1022. Full text: https://medicinainternaelsalvador.com/wp-content/uploads/2018/09/the_migraine_aura.5.pdf
- Bickerstaff, E. (1961). Basilar artery migraine. The Lancet , 277 (7167), 15-17. Citation: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(61)92184-5/fulltext
- Kadian, R., & Kumar, A. (2019). Basilar Migraine. Full text: https://www.ncbi.nlm.nih.gov/books/NBK507878/
- Kumar, A., & Arora, R. (2019). Hemiplegic Migraine. Full text: https://www.ncbi.nlm.nih.gov/books/NBK513302/
- Shapiro, R. E. (2008). Caffeine and headaches. Current pain and headache reports , 12 (4), 311. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/18625110
- Edlow, A. G., & Bartz, D. (2010). Hormonal contraceptive options for women with headache: a review of the evidence. Reviews In Obstetrics And Gynecology , 3 (2), 55. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2938905/
- Ambrosini, A., d’Onofrio, M., Grieco, G. S., Di Mambro, A., Montagna, G., Fortini, D., … & Buzzi, M. G. (2005). Familial basilar migraine associated with a new mutation in the ATP1A2 gene. Neurology , 65 (11), 1826-1828. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/16344534
- Robbins, M. S., Lipton, R. B., Laureta, E. C., & Grosberg, B. M. (2009). CACNA1A nonsense mutation is associated with basilar‐type migraine and episodic ataxia type 2. Headache: The Journal of Head and Face Pain , 49 (7), 1042-1046. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/19486177
- Sharma, H. (2015). Meditation: process and effects. Ayu , 36 (3), 233. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895748/
- Kondo, M. C., Jacoby, S. F., & South, E. C. (2018). Does spending time outdoors reduce stress? A review of real-time stress response to outdoor environments. Health & place , 51 , 136-150. Full text: https://www.fs.fed.us/nrs/pubs/jrnl/2018/nrs_2018_kondo_004.pdf
- Lin, Y. K., Lin, G. Y., Lee, J. T., Lee, M. S., Tsai, C. K., Hsu, Y. W., … & Yang, F. C. (2016). Associations between sleep quality and migraine frequency: a cross-sectional case-control study. Medicine , 95 (17). Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4998727/
- Cervoni, C., Bond, D. S., & Seng, E. K. (2016). Behavioral weight loss treatments for individuals with migraine and obesity. Current pain and headache reports , 20 (2), 13. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/26862055
- Tuchin, P. J. (2008). A case of chronic migraine remission after chiropractic care. Journal of chiropractic medicine , 7 (2), 66-70. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2682939/
- Hou, M., Xie, J. F., Kong, X. P., Zhang, Y., Shao, Y. F., Wang, C., … & Hou, Y. P. (2015). Acupoint injection of onabotulinumtoxin A for migraines. Toxins , 7 (11), 4442-4454. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4663513/
- Robbins, M. S., & Blumenfeld, A. Peripheral Nerve Blocks for Headaches. Full text: https://americanheadachesociety.org/wp-content/uploads/2018/05/Andrew_Blumenfeld_and_Matthew_Robbins_-_Peripheral_Nerve_Blocks.pdf
- Sasannejad, P., Saeedi, M., Shoeibi, A., Gorji, A., Abbasi, M., & Foroughipour, M. (2012). Lavender essential oil in the treatment of migraine headache: a placebo-controlled clinical trial. European neurology , 67 (5), 288-291. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/22517298
- Borhani Haghighi, A., Motazedian, S., Rezaii, R., Mohammadi, F., Salarian, L., Pourmokhtari, M., … & Miri, R. (2010). Cutaneous application of menthol 10% solution as an abortive treatment of migraine without aura: a randomised, double‐blind, placebo‐controlled, crossed‐over study. International journal of clinical practice , 64 (4), 451-456. Abstract: https://www.ncbi.nlm.nih.gov/pubmed/20456191
- Pittler, M. H., & Ernst, E. (2004). Feverfew for preventing migraine. Cochrane database of systematic reviews , (1). Abstract: https://www.ncbi.nlm.nih.gov/pubmed/14973986
- Martins, L. B., Rodrigues, A. M. D. S., Rodrigues, D. F., dos Santos, L. C., Teixeira, A. L., & Ferreira, A. V. M. (2019). Double-blind placebo-controlled randomized clinical trial of ginger (Zingiber officinale Rosc.) addition in migraine acute treatment. Cephalalgia , 39 (1), 68-76. Full text: http://www.naturalhealthresearch.org/wp-content/uploads/2020/01/Ginger-Treatment-for-Acute-Migraine-Headache.pdf
The post Basilar Migraine: Triggers, Symptoms, Treatment & Prevention appeared first on Denver Upper Cervical Chiropractic.
Visit us at Denver Upper Cervical Chiropractic
We serve patients in Denver, CO.
HOURS
Monday 1:00 pm – 6:00 pm
Tuesday 9:00 am – 6:00 pm
Wednesday 1:00 pm – 6:00 pm
Thursday 9:00 am – 6:00 pm
Friday Reserved for Traveling Patients
1778 S Broadway, Denver, CO 80210, United States of America
Phone:
(303)-955-8270