Can Chiropractic Care Relieve Occipital Neuralgia Pain?
Occipital neuralgia (ON) is a distinct form of nerve pain that affects the occipital nerves running from the top of the spinal cord (near your occipital bone) up through the scalp.
Patients typically get this pain at the back of the head, sometimes radiating to the side of the head or upper neck. It’s often mistaken for migraines or other types of headache.
Chiropractic care, with its focus on the health of the spinal column and nervous system, offers relief from the chronic pain of occipital neuralgia. I’ll review how chiropractic treatment (especially upper cervical chiropractic ) addresses the root cause of occipital neuralgia.
What Does Occipital Neuralgia Feel Like?
Occipital neuralgia is characterized by intense pain that can feel like an electric shock in the upper neck, back of the head, and behind the ears. Often described as piercing and throbbing, this pain can be so severe that it mimics the sensation of a migraine headache . This pain is similar to that of trigeminal neuralgia but focused in a different area.
The symptoms of occipital neuralgia are unique because of where they occur. Most often, this pain radiates from the base of the skull, with pain that can move around the back of your head and sometimes involve the scalp.
It’s not just the intensity of the pain that sets ON apart, but also its sharp, jabbing nature, which can be sporadic or continuous. Many patients describe the pain as similar to touching a live wire or an ice pick being driven into their head.
What Causes Occipital Neuralgia?
Occipital neuralgia occurs when one or more of the occipital nerve roots (located at the top of your spinal cord) are inflamed or irritated. 90% of the time, occipital neuralgia happens when the largest of the nerves, the greater occipital nerve, is compressed (a pinched nerve) or inflamed.
To truly understand how this works, you must briefly understand occipital nerve stimulation.
Occipital nerves are a group of nerves from C2 to C3. There are 3 occipital nerves:
- Greater occipital nerve
- Lesser occipital nerve
- Third occipital nerve
There are several triggers that can lead to occipital neuralgia pain:
- Injury to the neck (such as whiplash)
- Muscle tightness
- Infection
- Gout
- Diabetes
- Tumors
- Blood vessel inflammation
- Cervical disc disease
- Arthritis of the upper cervical spine
- Nerve compression in the cervical spine
If your occipital nerves are already inflamed or irritated, touching the back of your head or neck may trigger occipital neuralgia. Even brushing your hair or bumping your head against a headrest may trigger it.
How Chiropractic May Help with Occipital Neuralgia
Upper cervical chiropractic care, also known as orthospinology , is uniquely good for occipital neuralgia treatment.
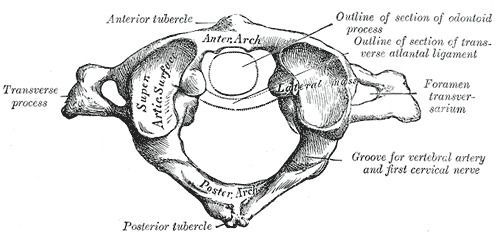
The occipital nerves run from the base of the brain and exit through C2. Upper cervical chiropractic adjustments zero in on the very top of your neck (vertebrae C1 and C2), where small misalignments can have a big impact on the occipital nerves.
When these top neck vertebrae aren’t aligned right, it can squeeze or irritate the nerves. That’s often what causes the sharp, severe pain of occipital neuralgia. Chiropractors like myself use precise techniques to gently address this dysfunction, which can ease the pressure on the nerves and, in turn, relieve the pain.
I frequently employ occipital lift adjustments and precise, individualized work on the atlas . Sometimes a simple, occipital lift adjustment works well — this adjustment gently creates a distractive force between the occiput and C1. But while occipital lift is more ‘popular,’ I find it to work less effectively for patients with occipital neuralgia.
An occipital lift is less precise and may not be achievable based on where you contact the patient. Many chiropractors can perform this adjustment type if they have the right table, but it lacks the finesse or precision of actual atlas work.
For many people with occipital neuralgia, focused atlas work is going to be the most probable route to relief.
This kind of chiropractic care isn’t just about nudging bones into the right place. It’s also about the overall health of your nervous system.
Adjustments in the upper neck can reduce swelling , improve blood flow, and help nerves work better. This can lessen the occipital neuralgia symptoms, from the intense, shock-like pain to the constant, dull ache.
Upper cervical chiropractic is gentle and doesn’t involve any harsh treatments. Many people with occipital neuralgia find that it significantly cuts down on how often and how badly they get these headaches, helping them get back to their daily activities without the burden of constant pain.
Other Treatments
In addition to upper cervical chiropractic care, there are several other non-invasive treatment options for managing occipital neuralgia. They focus on alleviating head and neck pain and reducing the frequency of headaches without the need for surgery or invasive procedures.
- Massage therapy: Massage helps relax tight muscles in the neck and upper back and can reduce muscle tension that might be compressing the occipital nerves. Even self-massage can help with ON pain.
- Acupuncture and dry needling: Recent research shows that both acupuncture and dry needling may improve clinical outcomes for occipital neuralgia patients. Dry needling is essentially acupuncture, but based entirely on peer-reviewed research from the past few decades.
- Physical therapy : These exercises and stretches can strengthen neck muscles. Physical therapy aims to improve posture and range of motion, reducing strain on the occipital nerves.
- Heat and cold therapy*: Applying heat can relax tight muscles and improve blood circulation. Then, cold packs can help reduce inflammation and numb pain. *This is most effective when used within the first 24-48 hours after an injury that caused ON pain.
- Over-the-counter pain relievers: Anti-inflammatory medication and pain relievers like ibuprofen or acetaminophen can be used for temporary pain relief. They can help you manage pain episodes and reduce inflammation. However, I recommend these only for the very short term, as taking pain relievers often may have negative effects on your overall health.
- Relaxation techniques: Techniques like deep breathing, meditation, or yoga can help manage stress. Stress reduction is key in preventing muscle tension that can trigger ON.
- Lifestyle adjustments: Ergonomic adjustments at work or home may help if your pain is triggered by poor posture and muscle tension. Ensuring proper neck support while sleeping or sitting can prevent strain on the neck.
Each of these treatments can be used alone or in combination with upper cervical chiropractic care for a comprehensive approach to managing occipital neuralgia.
Home Remedies
There are a few home remedies for occipital neuralgia. These are non-invasive, inexpensive, and side-effect-free. Effective home remedies for occipital neuralgia include:
- Rest
- Warm compress
- Self-massage
You may also want to try all-natural anti-inflammatories that may reduce inflammation in or around your occipital nerves.
Consider trying these all-natural anti-inflammatories in conjunction with seeking chiropractic care:
- Curcumin (turmeric)
- Cat’s claw
- Green tea
- Resveratrol
- Omega-3 fatty acids (fish oil)
- Capsaicin (chili pepper)
- Boswellia (AKA frankincense)
- White willow bark
- Maritime pine bark
How to Prevent Occipital Neuralgia
There are several ways to prevent inflammation or irritation of the occipital nerves that causes occipital neuralgia:
- Exercise and stretch regularly.
- Use good posture.
- Avoid holding your head in a downward position for long periods of time.
- If you experience muscle tension, try to relax the muscles and relieve the tension.
- If you have an infection, get it treated before it irritates the nerves in your upper spine.
- If you are injured in the neck area, seek medical attention to assess the damage.
If your occipital nerves are already inflamed or irritated, avoid touching the back of your head or neck, unless you have to. In that case, be very gentle.
FAQs
Occipital neuralgia is not a life-threatening condition but may lead to serious impacts on your job productivity, school performance, and overall quality of life. That’s why you should seek out treatment for occipital neuralgia if it flares up.
To diagnose occipital neuralgia, a doctor may perform the following:
- Symptoms checklist
- Medical history
- Family medical history
- Physical examination
- Ultrasound
- MRI
- CT scan
- Blood tests
- Nerve block
A doctor may inject an occipital nerve block into the affected area to diagnose occipital neuralgia. If the nerve block resolves your headache pain, then your occipital nerves are probably irritated or inflamed.
Doctors may also prescribe prescription drugs such as muscle relaxants, steroid injections, or antidepressants for occipital neuralgia. Muscle relaxants should relax the muscles around your occipital nerves, taking pressure off those nerves and offering occipital pain relief.
Anti-seizure meds, tricyclic antidepressants, and SSRIs (selective serotonin reuptake inhibitors) are all common prescription drugs used to treat occipital neuralgia. These all come with a laundry list of serious side effects, so it’s important to discuss these with your doctor before going this route.
Health care doctors may also administer injections to relieve occipital neuralgia. Since injections are more invasive than other treatments, these are often a last resort in the case that nothing else works.
Local anesthetic may be injected near the occipital nerves, bringing up to a year of occipital pain relief. (If you don’t treat the underlying cause, occipital neuralgia will likely return.)
A 2018 meta-analysis shows that botox (botulinum toxin) injections may be a safe and effective treatment for occipital neuralgia.
Surgical treatment attempts to correct several issues that may be triggering your occipital pain.
Occipital release surgery involves making small incisions to un-pinch occipital nerves. Sometimes, inflamed tissue needs to be incised to release pressure off of your occipital nerves, in order to prevent future occipital neuralgia attacks.
If your occipital nerves are compressed due to osteoarthritis or rheumatoid arthritis, surgery may be used to ease the nerve pressure. A ganglionectomy is a surgery meant to disrupt nerve clusters that may contribute to occipital pain.
Neurosurgeons may surgically place electrodes under your skin to stimulate the occipital nerves, or perhaps between your spinal cord and vertebrae. These electrodes are meant to block pain messages traveling through your nervous system.
In extreme cases, neurosurgery may sever the greater occipital nerve. This will lead to scalp numbness.
No, occipital neuralgia cannot be cured in the traditional sense. Pain can be managed, and attacks can be prevented. If you can figure out the underlying cause of your occipital neuralgia and treat it, you may be “cured” as long as the underlying cause does not recur.
You Don’t Have to Live in Pain — We Can Help
If you suffer from frequent headaches, consider upper cervical chiropractic care. At Denver Upper Cervical Chiropractic, we use evidence-based techniques to gently manipulate the spine. Most headache pain can be relieved with spinal adjustments.
Click here today to make an appointment with us!
- Korabelnikova, E. A., Danilov, A. B., Danilov, A. B., Vorobyeva, Y. D., Latysheva, N. V., & Artemenko, A. R. (2020). Sleep disorders and headache: A review of correlation and mutual influence. Pain and therapy , 9 (2), 411-425. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7648824/
- Elizagaray-Garcia, I., Beltran-Alacreu, H., Angulo-Díaz, S., Garrigos-Pedron, M., & Gil-Martinez, A. (2020). Chronic primary headache subjects have greater forward head posture than asymptomatic and episodic primary headache sufferers: Systematic review and meta-analysis. Pain medicine , 21 (10), 2465-2480. Full text: https://www.researchgate.net/profile/Ignacio-Elizagaray-Garcia-2/publication/345144818_Chronic_Primary_Headache_Subjects_Have_Greater_Forward_Head_Posture_than_Asymptomatic_and_Episodic_Primary_Headache_Sufferers_Systematic_Review_and_Meta-analysis/links/61c44cd7c99c4b37eb1878af/Chronic-Primary-Headache-Subjects-Have-Greater-Forward-Head-Posture-than-Asymptomatic-and-Episodic-Primary-Headache-Sufferers-Systematic-Review-and-Meta-analysis.pdf
- Fischer, M. A., & Jan, A. (2019). Medication-overuse headache. Full text: https://www.ncbi.nlm.nih.gov/books/NBK538150/
- Jovel, C. E., & Mejía, F. S. (2017). Caffeine and headache: specific remarks. Neurología (English Edition) , 32 (6), 394-398. Full text: https://www.sciencedirect.com/science/article/pii/S2173580817300858
- Leung, A. (2020). Addressing chronic persistent headaches after MTBI as a neuropathic pain state. The Journal of Headache and Pain , 21 (1), 77. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7304149/
- Kaur, A., & Singh, A. (2013). Clinical study of headache in relation to sinusitis and its management. Journal of Medicine and Life , 6 (4), 389. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3973877/
- Kikkeri, N. S., & Nagalli, S. (2022). Migraine with aura. In StatPearls [Internet]. StatPearls Publishing. Full text: https://www.ncbi.nlm.nih.gov/books/NBK554611/
- Ruschel, M. A. P., & De Jesus, O. (2023). Migraine headache. In StatPearls [Internet]. StatPearls Publishing. Full text: https://www.ncbi.nlm.nih.gov/books/NBK560787/
- Al Khalili, Y., & Chopra, P. (2020). Hypnic Headache. Full text: https://www.ncbi.nlm.nih.gov/books/NBK557598/
- Arca, K. N., & Halker Singh, R. B. (2019). The hypertensive headache: a review. Current pain and headache reports , 23 , 1-8. Full text: https://www.iranheadache.ir/wp-content/uploads/2020/04/The-Hypertensive-Headache-a-Review.pdf
- Jersey, A. M., & Foster, D. M. (2018). Cerebral aneurysm. Full text: https://www.ncbi.nlm.nih.gov/books/NBK507902/
- Vernon, H., Borody, C., Harris, G., Muir, B., Goldin, J., & Dinulos, M. (2015). A randomized pragmatic clinical trial of chiropractic care for headaches with and without a self-acupressure pillow. Journal of manipulative and physiological therapeutics , 38 (9), 637-643. Abstract: https://pubmed.ncbi.nlm.nih.gov/26548737/
- Al Khalili, Y., Ly, N., & Murphy, P. B. (2018). Cervicogenic headache. Full text: https://www.ncbi.nlm.nih.gov/books/NBK507862/
- Urits, I., Patel, M., Putz, M. E., Monteferrante, N. R., Nguyen, D., An, D., … & Viswanath, O. (2020). Acupuncture and its role in the treatment of migraine headaches. Neurology and therapy , 9 , 375-394. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7606388/
- Jimenez, M. P., DeVille, N. V., Elliott, E. G., Schiff, J. E., Wilt, G. E., Hart, J. E., & James, P. (2021). Associations between nature exposure and health: a review of the evidence. International Journal of Environmental Research and Public Health , 18 (9), 4790. Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8125471/
The post Can Chiropractic Care Relieve Occipital Neuralgia Pain? appeared first on Denver Upper Cervical Chiropractic.
Visit us at Denver Upper Cervical Chiropractic
We serve patients in Denver, CO.
HOURS
Monday 1:00 pm – 6:00 pm
Tuesday 9:00 am – 6:00 pm
Wednesday 1:00 pm – 6:00 pm
Thursday 9:00 am – 6:00 pm
Friday Reserved for Traveling Patients
1778 S Broadway, Denver, CO 80210, United States of America
Phone:
(303)-955-8270