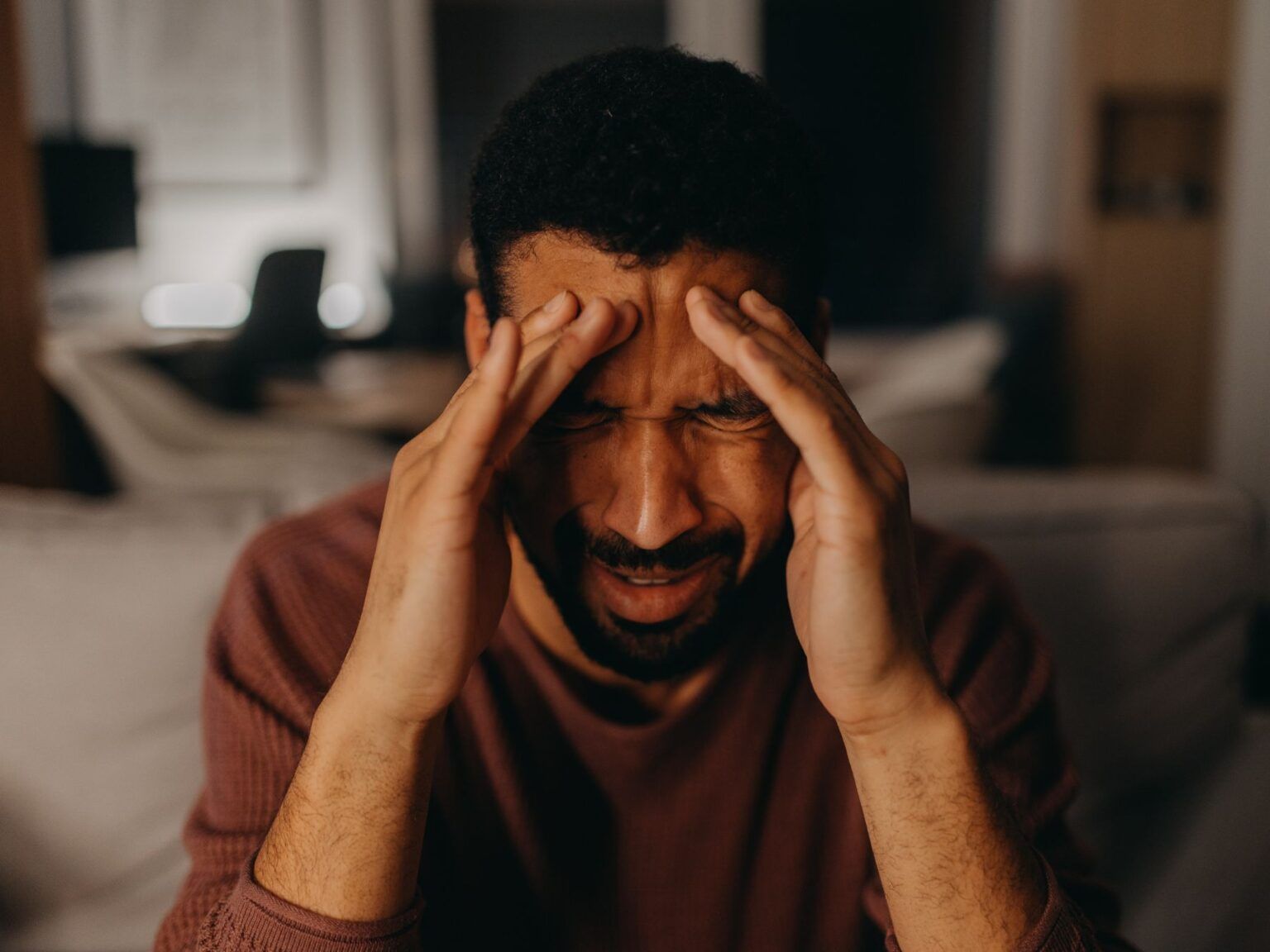
Headache
Headache Articles
Visit us at Denver Upper Cervical Chiropractic
We serve patients in Denver, CO.
HOURS
Monday 1:00 pm – 6:00 pm
Tuesday 9:00 am – 6:00 pm
Wednesday 1:00 pm – 6:00 pm
Thursday 9:00 am – 6:00 pm
Friday Reserved for Traveling Patients
1778 S Broadway, Denver, CO 80210, United States of America
Phone:
(303)-955-8270